Functionality has been added to the Diamond System to help our clients meet the reporting requirements of Section 111 Liability Insurance (include Self-Insurance), No-Fault Insurance and Workers’ Compensation. This Help File is designed to provide information on what is provided in the Diamond System. All clients should familiarize themselves with the reporting requirements and guidelines provided by the CMS (Center for Medicare and Medicaid Services).
This can be found at the following link: www.cms.hhs.gov/MandatoryInsRep.
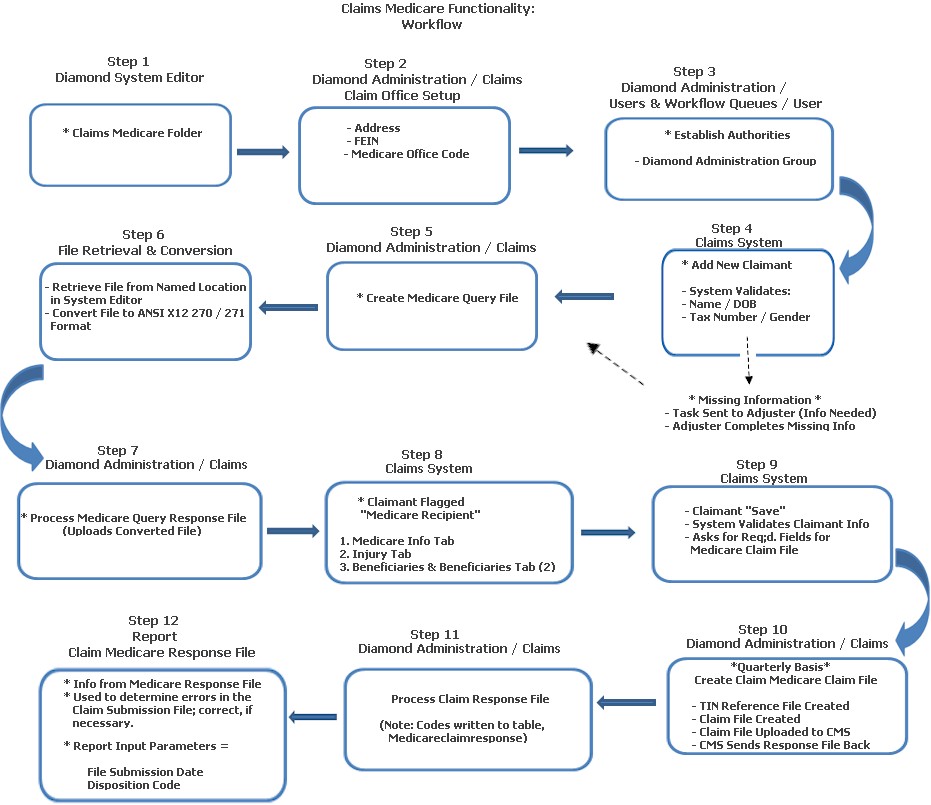
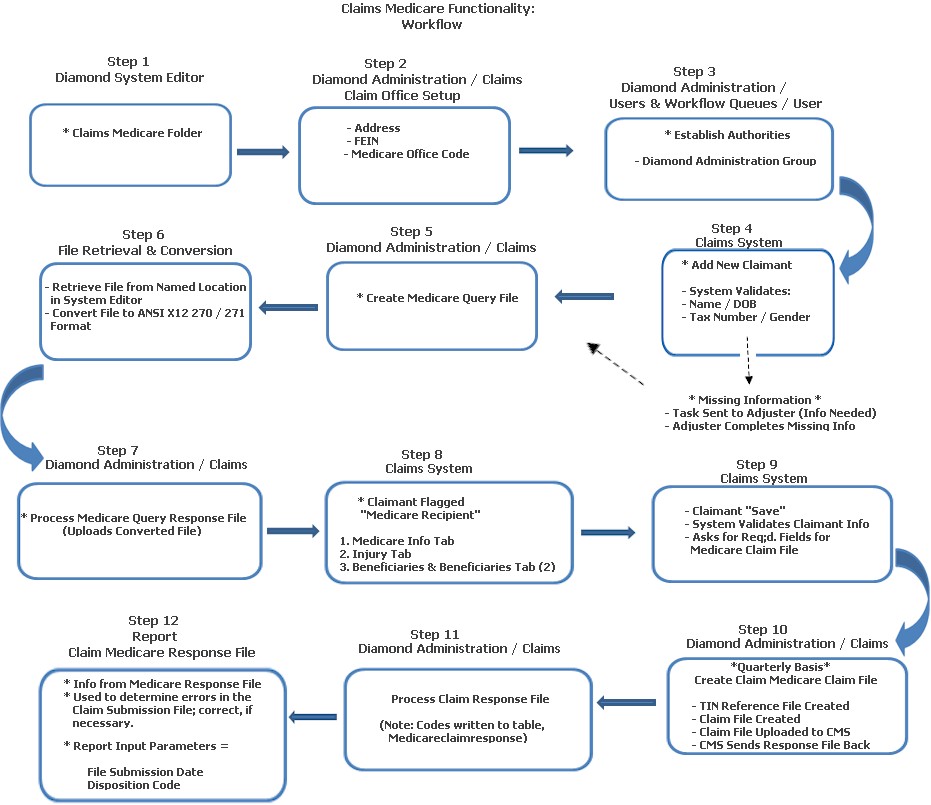
The diagram below represents how the Medicare functionality works in the Diamond System.
RRE ID
In order to report data to the CMS, each company is required to obtain an RRE ID by registering to report. This RRE ID must be entered in the system setting, “RRE ID,” in the Diamond System Editor in the Claims / Medicare folder. This ID will be used in the creation of the query and claim files and is required before any files can be created.
Output Path
Clients must also specify the output path for the query file and the claim file. This is a user defined / implementation specific system setting, “Output Path,” that is also located in Diamond System Editor in the Claims / Medicare folder.
Once the user has updated the system settings, the claim offices used for the claim personnel must be updated. The address and FEIN information that is used in the claim file is pulled from the claim office associated with the claim. Address and FEIN information can be the same for all claim offices, but they do give companies the options to allow different locations (for correspondence). A new option, Claim Office Setup, has been added to Diamond Administration to allow companies to add / update claim office information.
To access Claim Office Setup:
Open Diamond from your desk top
Right click the Diamond Agent caution sign in the right corner
From the pop up menu, click Administration / Claims / Claim Office Setup
On the Claim Office Setup screen, the user has the option to add / edit claim offices. To add the needed Medicare information (address and FEIN) for the office:
Highlight the office
Click Edit
On the Maintenance screen:
Enter the address of the office
Select FEIN from the combo box and enter the Federal ID number
The user can also supply a Medicare Office Code. This code was added by CMS to allow the company to associate claims with a different mailing address but the same FEIN. (Note: Please see the CMS user guide for further definitions of this field.)
When finished, click Save to retain your entries.
Special Note! Before creating any files, each company will also need to identify the coverages that have Medicare liability. Once these coverages have been identified, Insuresoft will deliver a script to update the medicare_liablity field in the Coverage Code Version table. This is very important, because the query file will only request the status on claimants added after the reporting date (01/01/2010) or prior to that date if they have an open loss reserve on Medicare liability coverage.
The last set up item that clients must do is assign authorities. These authorities should be assigned to the users responsible for creating the query and claim files and processing the response files from CMS. The new authorities are in the Diamond Administration group of authorities.
These, and their functions, include:
Claims Create Medicare Claim File: Allows a user to access the Create Medicare Claim File function in Diamond Processes. On a quarterly basis, each client will be required to submit a claim file to CMS. This process creates two (2) files: TIN (Tax ID Number) Reference and a Claim file that includes records that have been added, updated or deleted.
Claims Create Medicare Query File: Allows a user to access the Create Medicare Query File function in Diamond Processes. This process gathers any claimants added after 01/01/2010 or those that were added after 12/05/1980 and have open loss reserves that have not already been identified as a recipient.
Claims Process Medicare Query Response: Allows a user to access the Process Medicare Query Response function in Diamond Processes. This process reads the query response file from CMS, updates the Medicare HICN number and sets the recipient field for the claimant.
Process Medicare Claim Response File: Allows a user to access the Process Medicare Claim Response File function in Diamond Processes. This process transfers the disposition codes into the Medicareclaimresponse table.
Once the set up has been completed, clients can begin to create files and capture information for Medicare reporting requirements. The following section outlines what functionality is available in Diamond.
When a new claimant is added, the system validates if the information required for reporting in the Medicare Query file has been supplied. This includes the name, birth date, tax number and gender. If any of this information is not supplied, a task is sent to the adjuster on the claim indicating that information needed for the Medicare Query is missing. It is the adjuster’s responsibility to obtain the needed information.
Note: Please see the CMS user guide for further explanation on what information combinations are acceptable for CMS to identify a claimant as a Medicare recipient.
To access Create Medicare Query File:
Open Diamond from your desk top
Right click the Diamond Agent caution sign in the right corner
Click Administration on the pop up menu
Select Claims / Create Medicare Query File to generate the CMS Query file
When the user runs this process, the system does the following:
It gathers any claimants that have been added after 01/01/2010 or that were added after 12/05/1980 and have open loss reserves and that have not already been identified as a Medicare recipient.
Information from these claimants is used to create the query file that can be submitted to CMS to determine if the claimant is a Medicare recipient.
Once the file has been generated, the user needs to retrieve the file from the system setting location (defined above) and convert the file to ANSI X12 270/271 format. During registration you can indicate to use the HEW software provided by CMS.
Note: Please see the CMS user guide for additional information on the HEW Software.
After the file has been converted, it needs to be uploaded to the CMS Web Site for processing. When they have completed processing the file, a query response file is supplied to the client. This file needs to be converted back to a text file (use the HEW Software) and then processed in Diamond.
To process the response file:
Open Diamond from your desk top
Right click the Diamond Agent caution sign in the right corner
Click Administration on the pop up menu
Select Claims / Process Medicare Query Response File
On the Medicare Query Response screen, the user can then browse to the converted text file and select Process Query Response File.
During this process:
Diamond reads the response file and updates the Medicare HICN number.
It sets the Medicare recipient field for the claimant. (Please Note: This is done by tax number so if you have the same claimant on multiple claims, all claimants will be updated.)
Medicare Info Tab: Once the claimant has been flagged as a Medicare recipient, a new tab, “Medicare Info,” is available in the Claims System on the claimant for capturing the data needed for the CMS claim file. The Medicare Info tab contains several sub tabs for data capture. The main tab captures basic information for the claim file. Each field contains a definition (from the CMS user guide) to help the user understand what information should be supplied.
Injury Tab: The Injury tab captures data specific to the injury including the ICD-9 Diagnosis Codes.
Beneficiaries and Beneficiaries (2) Tabs: The Beneficiaries and Beneficiaries (2) tabs contain the information of a beneficiary receiving benefits in the case of a deceased Medicare recipient. The second Beneficiary tab allows you to enter two (2) additional beneficiaries.
Diamond clients should familiarize themselves with the information that can be submitted with the claim file and the requirements of CMS so that they are supplying the proper data.
When a claimant that has been identified as a Medicare recipient, additional validation has been added when saving the claimant. This validation will ask for the fields required for the Medicare Claim File being added if there is missing information.
On a quarterly basis, each client will be required to submit a claim file to CMS. This file is generated in Diamond Processes:
Open Diamond from your desk top
Right click the Diamond Agent caution sign in the right corner
Click Administration on the pop up menu
Select Claims / Create Medicare Claim File
When the Medicare Query Response screen returns, enter a file submission date (Note: This date is used as the file submission date in the claim file).
Select Create Claim File.
The Create Claim File process creates two (2) files:
The first file is a TIN Reference file that must be submitted anytime there is a change in the reporting TIN which includes the initial submission. Diamond generates this file whether or not a TIN is changed. The client does not need to submit the TIN Reference file unless changes were made. Please note that if you do not submit the file and there were changes to the TIN numbers that the claim records with the undefined TIN will be rejected.
The second file that is created is the claim file. This file includes records that have been added, updated and / or deleted required for the CMS reporting. Only records with valid data are reported. If basic claimant information has not been completed, the records are not reported. It is the responsibility of the client to complete the needed CMS information prior to creating the claim file.
In Step 10, once the Claim File is uploaded to CMS, CMS then sends a response file back. This function transfers the Disposition Codes to the Medicareclaimresponse table.
Open Diamond from your desk top
Right click the Diamond Agent caution sign in the right corner
Click Administration on the pop up menu
Select Claims / Process Claim File Response
Click Browse and select the directory / file location.
Click Open.
Select Process Claim Response File.
This report displays the information processed from the Medicare response file for a specific file submission date. The report can be filtered by disposition so that the user can only return data that is specific to failed records. This report should be used to determine errors in the Claims Submission file so that they can be corrected in the upcoming file submission.
Input parameters are:
File Submission Date
Disposition Code
Two (2) other Base System reports have been added for use with the new Medicare functionality in Diamond. These include the following:
Claimant Without Medicare Info By Date: This report returns any claimants added to the system after the supplied date that do not have the information needed for the Medicare Secondary Payer Query. This includes name, social security number, birth date and gender. Input parameters are: company, state and line of business.
Claimant Without Medicare Info Open Coverage: This report returns any claimants that have open loss reserves on a coverage that has been identified as a Medicare reportable coverage and do not have the information needed for the Medicare Secondary Payer Query. This includes name, social security number, birth date and gender. Input parameters are: company, state and line of business.